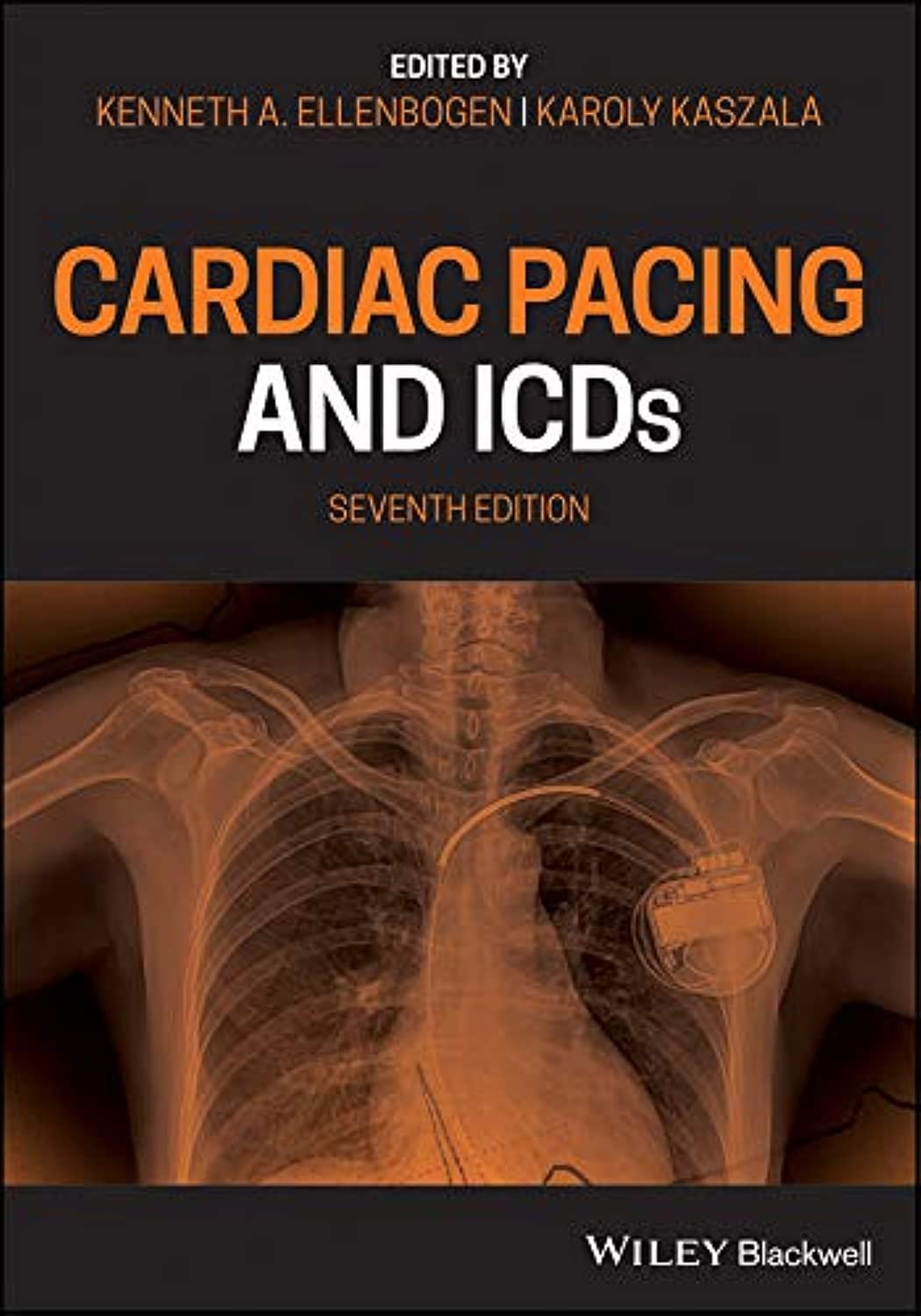
Cardiac Pacing and ICDs 7E PDF
Introduction
Cardiac Pacing and ICDs 7E PDF is a comprehensive guide for clinicians managing patients with rhythm disorders requiring pacemakers or implantable cardioverter-defibrillators (ICDs). These devices are critical for treating bradyarrhythmias, tachyarrhythmias, and preventing sudden cardiac death. According to the American Heart Association (AHA), timely device implantation and proper programming significantly improve patient outcomes. This manual offers practical strategies for device selection, implantation, programming, and long-term follow-up.
Principles of Cardiac Pacing
Types of Pacemakers
Pacemakers are categorized by chamber involvement and pacing mode. Single-chamber pacemakers stimulate either the atrium or ventricle, whereas dual-chamber devices coordinate atrial and ventricular contractions. Selecting the appropriate device depends on the patient’s rhythm disorder and underlying cardiac condition.
Indications for Pacemaker Therapy
Patients with symptomatic bradycardia, sinus node dysfunction, or atrioventricular block benefit from pacemaker implantation. Early intervention helps prevent syncope, heart failure progression, and improves quality of life.
Implantable Cardioverter-Defibrillators (ICDs)
ICD Function and Indications
ICDs continuously monitor cardiac rhythm and deliver shocks or pacing therapy to terminate life-threatening ventricular arrhythmias. Patients with prior sudden cardiac arrest, sustained ventricular tachycardia, or severe cardiomyopathy are prime candidates for ICD therapy.
Device Programming and Optimization
Programming involves adjusting detection thresholds, pacing rates, and therapy zones. Proper optimization reduces inappropriate shocks and ensures effective treatment. Regular follow-up and remote monitoring are essential for maintaining device performance and patient safety.
Complications and Risk Management
Device-Related Complications
Potential complications include lead dislodgement, infection, or device malfunction. Clinicians should monitor devices closely and intervene promptly to prevent adverse outcomes.
Arrhythmia Management
Despite device therapy, patients may develop arrhythmias requiring medication adjustment, ablation, or reprogramming. Timely intervention helps prevent hospitalizations and improves prognosis.
Long-Term Follow-Up
Patients need lifelong monitoring for device function, battery status, and cardiac health. Regular evaluations allow early detection of changes in rhythm or device performance.
Lifestyle and Patient Education
Educating patients on device function, activity restrictions, and warning signs is crucial. Compliance with follow-up schedules and medication regimens optimizes outcomes.
Conclusion
Cardiac pacing and ICD therapy are essential for managing arrhythmias and preventing sudden cardiac death. Early implantation, individualized device programming, and active follow-up ensure patient safety and quality of life.
👉 Download Cardiac Pacing and ICDs 7E PDF to access clinical protocols, case studies, and evidence-based strategies for device management.
🌐 For authoritative guidance, visit the American Heart Association (AHA) and Heart Rhythm Society.